4)Depression after a stroke
How many older people developed depressive symptoms or depression after a stroke and why?
If you click on an underlined word, it will take you to the glossary. From here you can scroll to the definition.
Quick-read Summary
- Previous work has shown that stroke-sufferers are more likely to develop depressive symptoms (feelings of low mood but not severe enough to be called depression) or depression.
- The aim was to find out how many stroke sufferers developed depressive symptoms or depression over 10 years and why.
- We found that suffering a stroke did infact increase the chance of developing depressive symptoms and depression and this increased with time.
- We found that people who had risk factors such as: cardiovascular risk factors, dementia and problems looking after themselves in daily living, had a higher chance of suffering with depressive symptoms.
Aims for the study
The aim was to find how many older stroke survivors developed depressive symptoms or depression over 10 years, and why. Depressive symptoms are common; an example would be the low mood we experience after a loved one dies. If depressive symptoms progress to become severe and significantly affect our ability to cope in life, this is called depression. Depression usually needs treatment with counselling or tablets.
Why did we do this study?
Previous research has shown that you are more likely to develop depression after a stroke. Research has suggested that cardiovascular risk factors increase risk of developing depression. We would like to do this research to find out if cardiovascular risk factors do increase the risk of depression.
What we did
We followed 355 stroke survivors over the age of 75 from 3 months to 10 years post-stroke.
There were a number of ways that we could find risk factors in these stroke survivors.
1) We looked at the medical history for every stroke survivor taking part.
2)We used the Bristol Activities of Daily Living Scale to measure stroke survivor's ability to carry out daily tasks, such as dressing and feeding.
3)We did a brain function test, called a 'Cambridge Cognitive Examination' (CAMCOG) on every person soon after their stroke. This measures brain function.
4)We did a blood test on every person to look for a specific form of a gene (APOE e4). It is a known cardiovascular risk factor.
5) We tested to look for depressive symptoms or depression. The stroke sufferer was asked a series of questions about their mood. This was repeated every year for ten years.
These were the cardiovascular risk factors we looked at:
- Age
- Gender
- Anti-depressants (drugs used to treat depression)
- Previous stroke
- Heart disease
- Atrial Fibrillation (an irregular heart beat)
- Diabetes
- High levels of cholesterol
- Blood vessel disease
- Smoking
- APOE ε 4
We also looked at a brain test (CAMCOG) score, this is a risk factor but is not a cardiovascular risk factor.
What did we find?
There were a few important relationships found in this study. This study found that those with a lower CAMCOG score were at a higher risk of developing depressive symptoms.
There was also a link between time and the development of depressive symptoms and depression. The graph below shows the development of depressive symptoms over time in the people from this study.
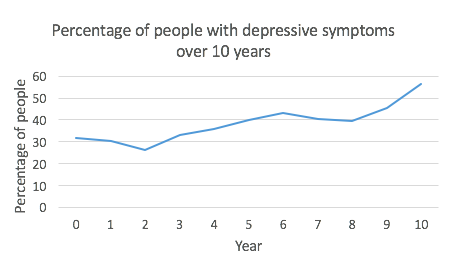
Overall, the graph appears to show that the number of people with depressive symptoms increased over time. Depression (more serious depressive symptoms that usually need counselling or tablets) also increased over time but not nearly as much as depressive symptoms.
We also found that there was a link between people with depressive symptoms and certain risk factors.
The following risk factors increased a stroke sufferers chance of developing depressive symptoms:
- Lower brain function (in comparison to a normal level for that age)
- Dementia
- Problems looking after themselves
- Cardiovascular risk factors
Key message: What can you do to lower your risk of depression after a stroke?
A stroke can cause major losses of bodily functions which can cause problems with daily living. Life can become a struggle and as a result many people experience depressive symptoms, which can progress to depression (a term used by doctors for people who feel very low in mood for long periods of time).
In simple terms, you can feel like giving up because life becomes very difficult. It is really important to realise that there are many changes which can improve your mood. It is easy to feel that you cannot be helped anymore but this is rarely the case.
Your GP can help you with this in many ways. It may be helpful for you to do a depression test before seeing your GP. You can find your score by doing a short online test. Click here to take the test.
It will give you a score which you could take to your GP appointment as a good starting point to discuss how your low mood is affecting your life. If you are a relative or carer for somebody, and you have noticed that their mood has changed, especially after a stroke, you should encourage them to speak to their doctor. Depression is a risk factor for developing dementia. You will find more information about depression under the tab ‘Risk factors for dementia and stroke’.
There are lots of way that doctors can help with depression but there are also changes you can do yourself. This study found that cardiovascular risks increase our chance of developing depression after a stroke. To lower the cardiovascular risks found in this study, you can:
- Eat healthily; eat plenty of fruit and vegetables
- Give up smoking
- Exercising your brain (puzzles and reading).
At the moment the NHS does not test for this APOE e4 allele as we do not have treatments for it. In the future, if treatments do become available then we can test for this allele and try to help lower peoples risk of developing dementia.
If you would like to more about depression, please click here