About Our Research
ADMISSION will lay foundations for new approaches to the recognition and treatment of multiple long-term conditions (MLTC) in hospital and inform the design of future care, with potential to improve health outcomes for the millions of patients with MLTC admitted to hospital each year.
A key part of ADMISSION is our partnership with patients and public with whom we have worked closely, since its inception, to design and develop our research. The Collaborative brings together experts in many disciplines including data science, advanced statistical methods, social science and genetic epidemiology. It also includes clinical researchers from secondary care who specialise in managing hospitalised patients with MLTC as well as researchers from primary care and public health. By utilising patient record data across UK Global Digital Exemplar hospitals together with HDRUK Acute Care Hub data science expertise we aim to build a data platform to capture the burden, inequalities and patient pathways for different multimorbidity clusters.
Work packages
ADMISSION is divided into five scientific work packages, with patient and public involvement and research capacity development underpinning all areas of the project.
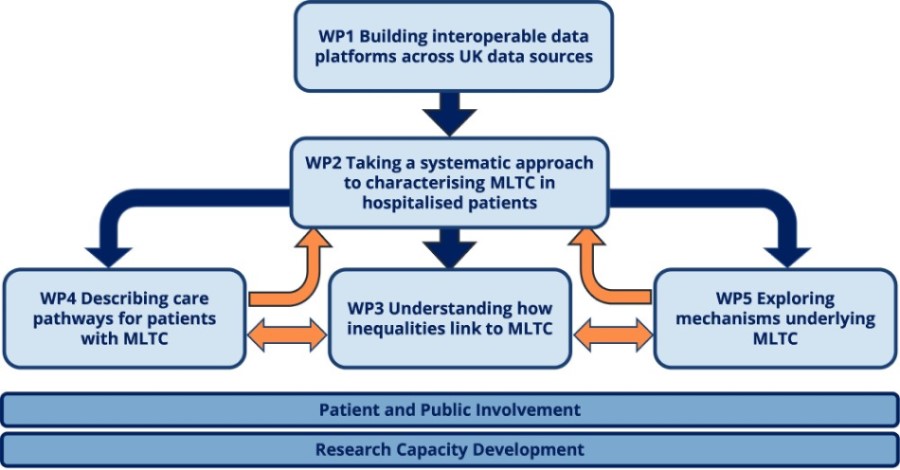
Work Package 1 aims to build an aligned, curated, interoperable data platform containing routinely collected data from hospitalised patients across the acute care pathway. This will be achieved by deriving the data from routinely-collected healthcare datasets necessary to undertake the work of the ADMISSION Research Collaborative. The end product of WP1 will be a set of three aligned, curated data platforms (one from Newcastle Hospitals electronic health record, one from the PIONEER HDRUK data source, and one from the UCLH). In addition, we will align diagnoses with those available in cohorts including UK Biobank to facilitate comparisons across multiple datasets.
Work Package 2 aims to take a systematic approach to characterising multiple long-term conditions (MLTC) in hospitalised patients. It will examine burden and patterns of MLTC in patients admitted to hospital through a series of complementary methods. We will use data from the routinely-collected sources curated in WP1, alongside data from large population-based studies including UK Biobank.
Work Package 3 will investigate key drivers of inequality in multiple long-term conditions in hospitalised patients and explore their impacts on healthcare pathways and outcomes. We will focus on how age, sex, ethnicity and socioeconomic deprivation contribute to the occurrence of MLTC in hospitalised patients and will explore the impact of drivers of inequality on healthcare pathways and outcomes. To complement quantitative analyses of routinely collected data, we will also conduct focused qualitative work involving in-depth interviews with a purposive sample of people with recent experience of hospitalisation.
Work Package 4 aims to map patterns of conditions in the context of patient pathways to understand hospital-based health service use, antecedent events and consequences after admission. We will map how patterns of conditions identified in WP2 influence experiences of delivery of care and care pathways across the acute care journey using quantitative and qualitative methods.
Work Package 5 aims to gain novel insights into the biological mechanisms which underpin multiple long-term conditions. This work will be conducted in two phases:
Phase One: Genetic epidemiology approaches in UK Biobank to understand mechanisms such as inflammation, oxidative stress, cortisol and telomere length. Phase Two: Phenotypic confirmation of candidate mechanisms using biobanked samples from SHARE – the Scottish Health Register and Biobank.
